The itch-scratch cycle
Itching and scratching can exacerbate each other. Scratching provides temporary relief as pain overrides the itch, but the damage to the skin leads to an inflammatory response, resulting in increased itching.
In addition to many individual triggers such as sweating, climatic conditions, heating air, wool, skin dryness, or an allergic reaction, stress can also intensify this vicious cycle, known as the ‘itch-scratch cycle.
Stress can come into play at any point in this cycle and exacerbate it:
Anti-inflammatory treatment
The primary approach to the medical treatment of itching, in addition to proper and consistent skin care using non-active base therapies to counteract skin dryness, involves the topical application of anti-inflammatory creams or ointments to inflamed areas of the skin.
When used sensibly, the benefits of anti-inflammatory agents (glucocorticoids [corticosteroids], calcineurin inhibitors) far outweigh the potential disadvantages. Abstaining from them can be as harmful to the skin as irresponsible usage.
Measures used in the therapy against itching:
- Basic Therapy
- Topical (externally applied) Calcineurin Antagonists
- Topical Glucocorticoids (Corticosteroids)
- Polidocanol
- Tannins
Antihistamines
There is actually no scientific evidence from studies to support the idea that taking antihistamines is helpful in relieving itching in atopic dermatitis.
In very rare individual cases, the use of antihistamines may be of benefit, but it should not be regular and over an extended period. Antihistamines with a sedative effect can impact sleep quality.
The Commission for Drug Safety in Childhood (KASK) of the German Society for Pediatric and Adolescent Medicine (DGKJ) advises against the use of certain over-the-counter sedating antihistamines (e.g., Doxylamine, Diphenhydramine, Dimenhydrinate [Diphenhydramintheophyllinate], Promethazine) due to a very unfavorable benefit-risk profile.
Non-pharmacological strategies against itching
For alleviating itching, physical and behavioral therapeutic measures can also be very successful:
- Cooling
- Skincare with cooling creams, lotions, or sprays
- Compresses with black tea
- Fatty-moist dressings
- Scratch alternatives such as tapping or pinching on adjacent non-inflamed areas
- Distraction and relaxation (music, autogenic training, etc.)
Detailed instructions on skincare, compresses, and dressings can be found in the chapter on care.
Regular documentation of the skin condition using ‘PO-SCORAD’
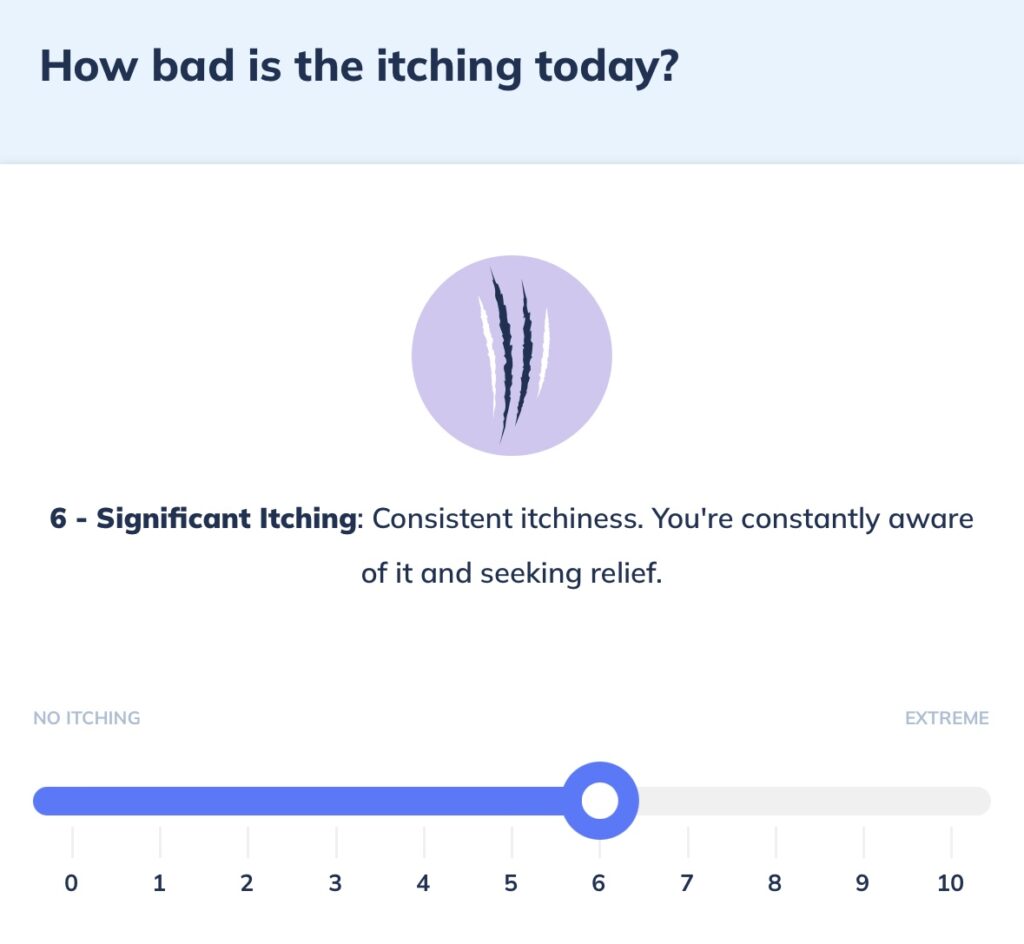
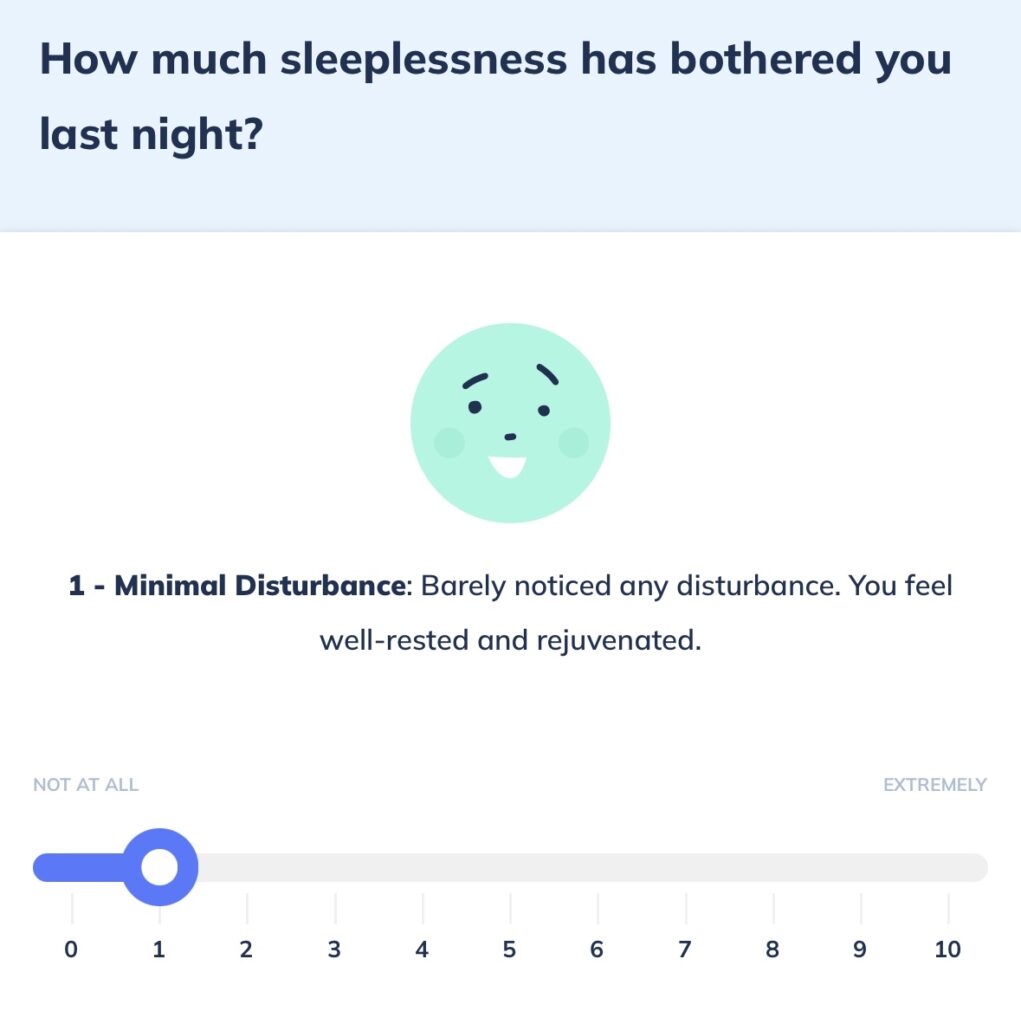
To more accurately assess whether and which of the many measures have been most helpful for your child, it is often helpful to collaborate with your doctor and utilize your expertise as a parent. To present a more objective evaluation of the skin and better contextualize it in the doctor-patient interaction, the visual scale of the subjective PO-SCORAD can be beneficial. It helps monitor the effectiveness of applied therapies, including itchiness and sleep disturbances. For documentation, you can use the Nia app with the “Skin Mood” function. Simply record the subjective value on a scale from 0 (no sleep disturbance or itchiness at all) to 10 (severe sleep disturbance/severe itchiness).
Through the “Skin Mood” function in the Nia app, you can document sleep quality and itchiness.
Sources:
- Monatsschrift Kinderheilkunde 2012
- S2k-Leitlinie „Neurodermitis“ 2016, www.awmf.org (external)

